 Understanding the Signs of Fatty Liver: What to Look For
Understanding the Signs of Fatty Liver: What to Look For
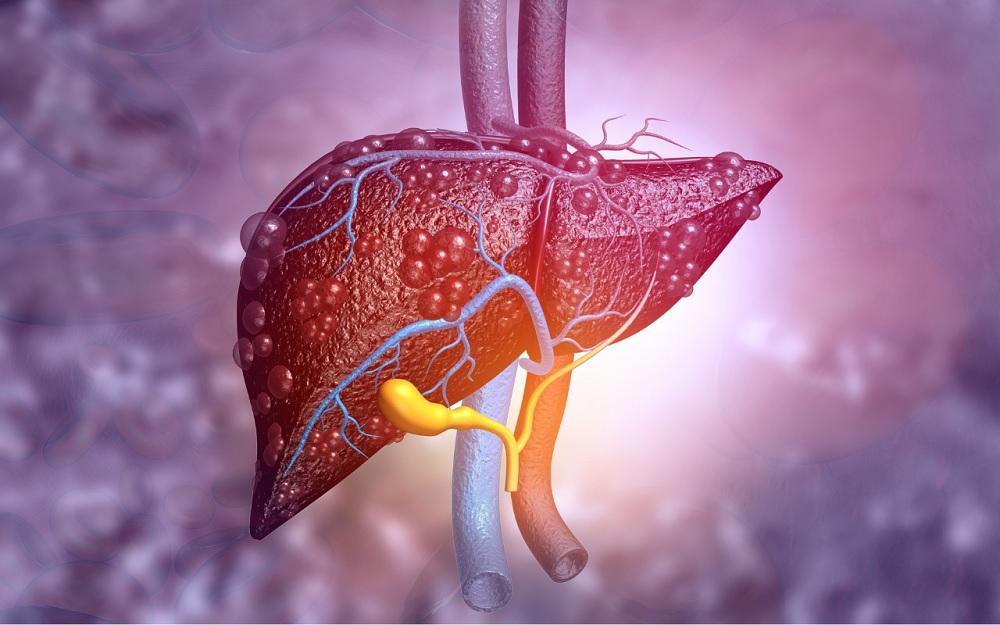
The liver is a remarkable organ that performs hundreds of essential functions in the body. From filtering toxins to aiding in digestion and metabolism, your liver works tirelessly to keep you healthy. However, when fat begins to accumulate in liver cells, it can lead to a condition known as fatty liver disease. This increasingly common health concern affects millions of people worldwide, yet many remain unaware they have it until the condition has progressed significantly.
What Is Fatty Liver Disease?
Fatty liver disease occurs when fat builds up in the liver cells. While it’s normal for the liver to contain some fat, when fat accounts for more than 5-10% of the liver’s weight, it’s considered a fatty liver. There are two main types of fatty liver disease:
Alcoholic Fatty Liver Disease (AFLD)
As the name suggests, this type results from excessive alcohol consumption. The liver prioritizes breaking down alcohol over other substances, leading to fat accumulation. Regular, heavy drinking can cause this condition, which can progress to more serious liver problems if alcohol consumption isn’t reduced or eliminated.
Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD occurs in people who drink little to no alcohol. It’s often associated with obesity, insulin resistance, high blood sugar, and high levels of fats in the blood. NAFLD is becoming increasingly prevalent worldwide, affecting an estimated 25-30% of adults in Western countries.
NAFLD can progress to non-alcoholic steatohepatitis (NASH), a more severe form that includes liver inflammation and can lead to scarring (fibrosis), cirrhosis, and even liver failure or liver cancer in some cases.
Common Signs and Symptoms of Fatty Liver
One of the most challenging aspects of fatty liver disease is that it’s often asymptomatic, especially in its early stages. Many people have fatty liver for years without realizing it, which is why it’s sometimes called a “silent disease.” However, as the condition progresses, several signs and symptoms may emerge:
Fatigue and Weakness
Persistent fatigue that isn’t relieved by rest can be one of the earliest signs of liver problems. The liver plays a crucial role in energy metabolism, and when it’s not functioning optimally, you may feel unusually tired or weak. This fatigue occurs because the liver struggles to remove toxins from the blood and process nutrients effectively.
Discomfort in the Upper Right Abdomen
The liver is located in the upper right portion of your abdomen, just below the ribcage. As fat accumulates and the liver becomes inflamed, you might experience a dull or aching pain in this area. Some describe it as a feeling of fullness or heaviness rather than sharp pain.
Unexplained Weight Loss
While fatty liver is often associated with obesity, some people with advanced fatty liver disease experience unexplained weight loss. This can occur when the liver loses its ability to process nutrients efficiently, leading to malnutrition despite adequate food intake.
Loss of Appetite
When the liver isn’t functioning properly, it can affect digestion and metabolism, leading to a reduced appetite. This symptom often accompanies nausea and can contribute to weight loss in advanced cases.
Nausea and Vomiting
Digestive disturbances such as nausea, vomiting, or stomach upset can occur as the liver’s ability to process food and remove toxins becomes compromised. These symptoms tend to be more common after meals, particularly those high in fat or protein.
Yellowing of Skin and Eyes (Jaundice)
Jaundice is a condition where the skin and whites of the eyes take on a yellowish tint. It occurs when the liver cannot process bilirubin (a yellow pigment formed from the breakdown of red blood cells) efficiently. While jaundice is more commonly associated with advanced liver disease and not typically an early sign of fatty liver, its appearance indicates significant liver dysfunction and requires immediate medical attention.
Spider-like Blood Vessels
Spider angiomas are small, spider-like blood vessels that can appear on the skin, typically on the chest, face, and arms. These occur due to imbalances in sex hormones resulting from the liver’s reduced ability to metabolize them properly. Like jaundice, spider angiomas are usually a sign of more advanced liver disease.
Swelling in the Legs and Abdomen
Edema (swelling in the legs and ankles) and ascites (fluid accumulation in the abdomen) can occur in advanced liver disease. These symptoms result from portal hypertension (increased pressure in the liver’s blood vessels) and reduced protein production, both consequences of significant liver damage.
Enlarged Liver or Spleen
As fat continues to accumulate, the liver can become enlarged (hepatomegaly). This might not be noticeable to you but can be detected during a physical examination by a healthcare provider. An enlarged spleen sometimes accompanies this as the body compensates for changes in blood flow through the liver.
Mental Confusion
In severe cases of liver dysfunction, toxins that would normally be filtered by the liver can build up in the bloodstream and affect brain function. This can cause confusion, difficulty concentrating, memory issues, and even changes in personality or sleep patterns – a condition known as hepatic encephalopathy.
Risk Factors for Developing Fatty Liver
Understanding risk factors can help identify those who might be more susceptible to developing fatty liver disease:
Obesity and Overweight
Excess body weight, especially around the midsection (central obesity), is strongly associated with NAFLD. Fat cells, particularly those in visceral fat, release inflammatory substances that can affect liver function and promote insulin resistance.
Insulin Resistance and Type 2 Diabetes
When cells become resistant to insulin, the pancreas produces more insulin to compensate. This excess insulin promotes fat storage in the liver. Approximately 70% of people with type 2 diabetes have some form of fatty liver disease.
High Cholesterol and Triglycerides
Elevated levels of triglycerides and LDL (“bad”) cholesterol, along with low levels of HDL (“good”) cholesterol, increase the risk of fat accumulation in the liver. This pattern of blood lipids, often called dyslipidemia, frequently occurs alongside other metabolic conditions.
Metabolic Syndrome
Metabolic syndrome is a cluster of conditions that occur together, increasing the risk of heart disease, stroke, and type 2 diabetes. These conditions include increased blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels. Having metabolic syndrome significantly increases the risk of developing NAFLD.
Excessive Alcohol Consumption
Regular consumption of large amounts of alcohol can lead to alcoholic fatty liver disease. For men, this typically means more than 14 drinks per week, and for women, more than 7 drinks per week. However, sensitivity to alcohol varies, and some people may develop liver problems with lower intake.
Rapid Weight Loss
While weight loss is generally recommended for overweight individuals with fatty liver, losing weight too quickly (more than 3-5 pounds per week) can actually worsen liver health temporarily. This occurs because rapid weight loss increases the amount of fat released into the bloodstream, some of which is taken up by the liver.
Certain Medications
Some medications can contribute to fatty liver development as a side effect. These include corticosteroids, certain chemotherapy drugs, some antibiotics, and medications used to treat conditions like heart rhythm disorders and inflammatory bowel disease. Never stop taking prescribed medications without consulting your healthcare provider.
Genetic Factors
Research suggests that genetic factors play a role in determining who develops fatty liver disease. Certain genetic variations affect how the body metabolizes fats and processes insulin, potentially increasing susceptibility to fat accumulation in the liver.
Diagnosing Fatty Liver Disease
Because fatty liver often doesn’t cause obvious symptoms, it’s frequently discovered during routine check-ups or while investigating other health concerns. The diagnostic process typically involves:
Medical History and Physical Examination
Your healthcare provider will ask about your medical history, including alcohol consumption, medication use, and family history of liver disease. They’ll also perform a physical examination, checking for an enlarged liver or other signs of liver dysfunction.
Blood Tests
Liver function tests measure levels of certain enzymes and proteins that can indicate liver inflammation or damage. Common tests include alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), and gamma-glutamyl transferase (GGT). While mildly elevated liver enzymes might suggest fatty liver, normal results don’t rule it out.
Imaging Tests
Ultrasound is typically the first imaging test used to detect fatty liver. It’s non-invasive and can show the characteristic bright liver tissue associated with fat accumulation. Other imaging options include computed tomography (CT) scans and magnetic resonance imaging (MRI), which can provide more detailed information about the amount of fat in the liver.
Liver Biopsy
Though less commonly used for initial diagnosis, a liver biopsy involves removing a small sample of liver tissue for examination under a microscope. This procedure can definitively diagnose fatty liver disease, determine its severity, and distinguish between simple fatty liver and more serious conditions like NASH or cirrhosis.
Managing and Treating Fatty Liver Disease
Currently, there are no approved medications specifically for treating fatty liver disease. Instead, management focuses on addressing underlying causes and making lifestyle modifications:
Weight Loss and Dietary Changes
For overweight individuals, losing 7-10% of body weight can significantly reduce liver fat and inflammation. Focus on a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Limit saturated fats, refined carbohydrates, and added sugars. Consider consulting a dietitian for personalized advice.
Regular Physical Activity
Exercise helps reduce liver fat even without significant weight loss. Aim for at least 150 minutes of moderate-intensity activity (like brisk walking) or 75 minutes of vigorous activity (like jogging) per week, along with muscle-strengthening activities twice weekly.
Limiting or Avoiding Alcohol
For those with alcoholic fatty liver disease, abstaining from alcohol is essential. Even for those with NAFLD, limiting or avoiding alcohol is advisable as it can exacerbate liver damage.
Managing Underlying Conditions
Treating conditions like diabetes, high cholesterol, and metabolic syndrome can improve liver health. Follow your healthcare provider’s recommendations regarding medications and monitoring for these conditions.
Avoiding Certain Medications
Some over-the-counter pain relievers like acetaminophen (Tylenol) can cause liver damage when taken in high doses or combined with alcohol. Always follow dosing instructions and discuss all medications with your healthcare provider.
Considering Coffee
Interestingly, moderate coffee consumption (2-3 cups daily) has been associated with a lower risk of liver disease progression. The protective effects may be due to coffee’s antioxidant properties and its ability to reduce inflammation.
When to See a Doctor
Consult a healthcare provider if you experience:
- Persistent fatigue or weakness
- Pain in the upper right abdomen
- Yellowing of the skin or eyes
- Swelling in the legs or abdomen
- Unexplained weight loss
- Confusion or personality changes
Additionally, consider screening for fatty liver if you have risk factors such as obesity, type 2 diabetes, or metabolic syndrome, even without symptoms.

Complications of Untreated Fatty Liver Disease
While many cases of fatty liver, particularly simple steatosis, don’t progress to more serious conditions, some cases can lead to:
Liver Inflammation (Steatohepatitis)
When fat accumulation is accompanied by inflammation, it’s called steatohepatitis (alcoholic steatohepatitis or non-alcoholic steatohepatitis, depending on the cause). This inflammatory state can damage liver cells and lead to fibrosis.
Liver Fibrosis
Persistent inflammation can cause scar tissue to form in the liver, a condition known as fibrosis. In early stages, fibrosis may be reversible with appropriate treatment and lifestyle changes.
Cirrhosis
Advanced fibrosis can lead to cirrhosis, where significant scarring impairs liver function. Cirrhosis increases the risk of liver failure and liver cancer and may eventually require liver transplantation.
Liver Cancer
Hepatocellular carcinoma (liver cancer) can develop in individuals with cirrhosis, though rarely in those with fatty liver without cirrhosis. Regular screening is recommended for those with cirrhosis.
Liver Failure
In severe cases, the liver may lose its ability to function, leading to liver failure. This life-threatening condition requires immediate medical attention and may necessitate liver transplantation.
Prevention of Fatty Liver Disease
Many of the strategies for managing fatty liver also help prevent its development:
Maintaining a Healthy Weight
Aim for a body mass index (BMI) in the normal range (18.5-24.9). If you’re overweight, even modest weight loss can reduce your risk of developing fatty liver.
Eating a Balanced Diet
Focus on a Mediterranean-style diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats like olive oil. Limit processed foods, added sugars, and saturated fats.
Exercising Regularly
Physical activity helps maintain insulin sensitivity and prevents fat accumulation in the liver. Incorporate both cardiovascular exercise and strength training into your routine.
Limiting Alcohol Consumption
If you drink alcohol, do so in moderation – up to one drink per day for women and up to two drinks per day for men. Consider abstaining completely if you have other risk factors for liver disease.
Managing Chronic Conditions
Keep conditions like diabetes, high blood pressure, and high cholesterol under control through medication, diet, exercise, and regular check-ups.
Conclusion
Fatty liver disease is a common condition that often progresses silently, potentially leading to serious liver complications if left unaddressed. By understanding the risk factors and recognizing potential signs and symptoms, you can take proactive steps to protect your liver health.
Remember that lifestyle modifications – particularly maintaining a healthy weight, eating a balanced diet, exercising regularly, and limiting alcohol consumption – are the cornerstones of both preventing and managing fatty liver disease. If you have risk factors or experience symptoms that might indicate liver problems, don’t hesitate to consult with a healthcare provider.
With early detection and appropriate management, the progression of fatty liver disease can often be halted or even reversed, preserving liver function and overall health for years to come. Your liver works tirelessly to keep you healthy – taking steps to protect it is one of the most important investments you can make in your long-term wellbeing.
